There’s a Way to Lower the Incidence of ADHD. We Should Try It.
Attention Deficit Hyperactivity Disorder (ADHD) is a name for a condition that includes tendencies to distraction and impulsive behavior. The condition has increased 30% in the last 10 years. Does that mean that Americans are almost a third more distractible than before, or has modern scientific medicine provided better tools for detecting traits that have been lurking in human populations all along? What prods these minds to distraction, and what are the best responses?
 Current research and approaches to
ADHD operate on a spectrum from the scientific to the social, with each of
these leanings emphasizing, respectively, ADHD as a problem beyond the human
normal to be diagnosed for bodily accuracy, and to be cured or at least
mitigated with pharmaceutical prescriptions, and ADHD as an extreme form of human
normal to be managed and even sometimes valued.
Current research and approaches to
ADHD operate on a spectrum from the scientific to the social, with each of
these leanings emphasizing, respectively, ADHD as a problem beyond the human
normal to be diagnosed for bodily accuracy, and to be cured or at least
mitigated with pharmaceutical prescriptions, and ADHD as an extreme form of human
normal to be managed and even sometimes valued.
Medical studies focus on the genetic and physiological role in the syndrome; they define the condition as a result of chemical imbalances, which result in behavior unusual, eccentric, or even anti-social. The focus of thinking is bodily, with the unwelcome behavior determined by the chemical physiology. The medical perspective has room for the role of the environment in that studies show ADHD worsened by unhealthy behavior, such as smoking or drinking of alcohol, especially among parents of prenatal and small children. Beyond this research on such environmental factors, there is little scientific understanding of the causes of the chemical imbalances. The center of the medical focus is on treatment, with pharmaceutical interventions to correct the imbalances. For many, this improves the ability to focus the mind’s executive function. Zoë Kessler, author of ADHD According to Zoë, testifies to the wonders of her medications. She received the diagnosis at age 47, and it came to her as a revelation explaining so many problems in her life; and the medications, with the mental focus she has gained, turned her life around. Although not a doctor, she speaks of the medical prescriptions for ADHD as progress out of recent Dark Ages, with untreated people suffering from constant distraction, and from all the social alienation that would follow.
By contrast, social interpretations look at the history of ADHD as the rise of a rigid formal measurement; in earlier times, societies more readily lived with social outliers. Now we call them abnormal with their conditions demarcated by medical labels and with need for drugs. The social perspective emphasizes recognizing, coping with, and healing from ADD, with suggestions for planning ahead for children easily distracted and appreciation for the different and sometimes extraordinary traits such children and adults sometimes possess. They hope for the kind of “neurodiversity” that Steven Silberman calls for in NeuroTribes, with appreciation for a spectrum of human mental life paralleling the spectrum thinking that has emerged for autism. Some M. D.s are urging just this change in thinking.
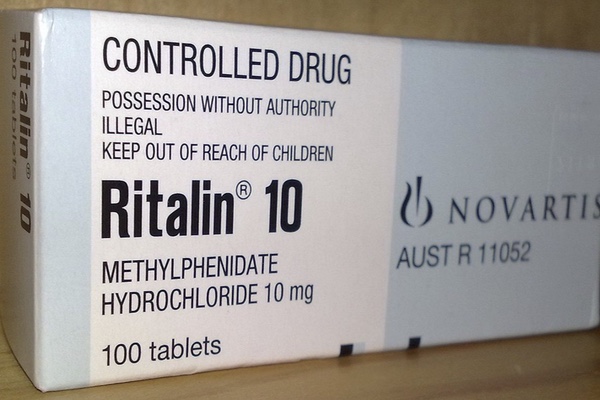
Pediatrician Dimitri Christakis, in his recent article, “Rethinking ADHD,” in the Journal of the American Medical Association, argues that all people are susceptible to distraction, and so, strictly speaking, everyone could benefit from the drugs currently prescribed for the condition. Indeed, there is a widespread informal economy of stimulant resale by average citizens dealing with stress; Ritalin, Vyvanse, Quillivant XR, and Adderall are particularly popular on college campuses at exam times. In the article, he acknowledges that tendencies to distraction begin with genetic predisposition, a context that justifies reliance on regular medication for many people, perhaps including Kessler. However, because those traits remain in place even with the pharmaceutical intervention, a whole range of challenges emerge about maintaining that medically induced internal correction. Patients can avoid full compliance, and when drugs wear off, problems multiply.
Although Christakis is a doctor, he is critical of the dominant medical perspective; so he considers the population-wide increase of medications excessive, even as he endorses the use of drugs in extreme cases. In particular, he urges moderation in pharmaceutical interventions; his position implies a call for more social tolerance of moderate differences in behavior, on the model of accepting differences in cultural background and physical ability. Construction of settings, especially in education, designed for clarity, can foster improvements in concentration. His medical and social advice brushes into moral commentary with his suggestion for changes in attitude. With shades of Ben Franklin’s homey advice and William James’s call for early habit formation, Christakis suggests personal discipline for taking on activities even when they do not spur much interest. Those acts of will power can cultivate the powers of attention, no matter one’s native endowment, and the ensuing patterns of resilience will pay dividends throughout life. That, he proposes, is the best remedy for many cases of ADHD and will lessen the need for pharmaceutical corrections. With inroads into medicine, the social interpretation of ADHD emphasizes prevention, while the medical model seeks solutions to deep-set problems.
The social approach to ADHD has a lot of curb appeal. It is less invasive; it coincides with acceptance of social diversity; and yet its emphasis on prevention can be difficult to achieve. Constructed setting to reduce distraction are wonderful; unplugging from devices that keep us on call constantly would help still more; and even tailoring ambitions more closely to one’s own resources and interests could further reduce the stress that spurs the distractions that the drugs are designed to remedy. Like pacifism, it would work best in ideal situations; yet these are ideals that have generally had little appeal in American culture. The conditions of recent history have been particularly ripe for the increase in ADHD diagnosis; the medical approach is well adapted to the way we live—as long as those standards remain the norm. We have the high degree of medical interventions that we deserve, and medical researchers and providers are responding to real needs once they have already emerged.
The challenge will be to find ways to make those ideals less idealistic, less out of reach. With some cultural changes reducing the enormity of distractions, prevention can become a realistic part of the response to ADHD—not for eliminating drug interventions, but to make them the tools of last resort.